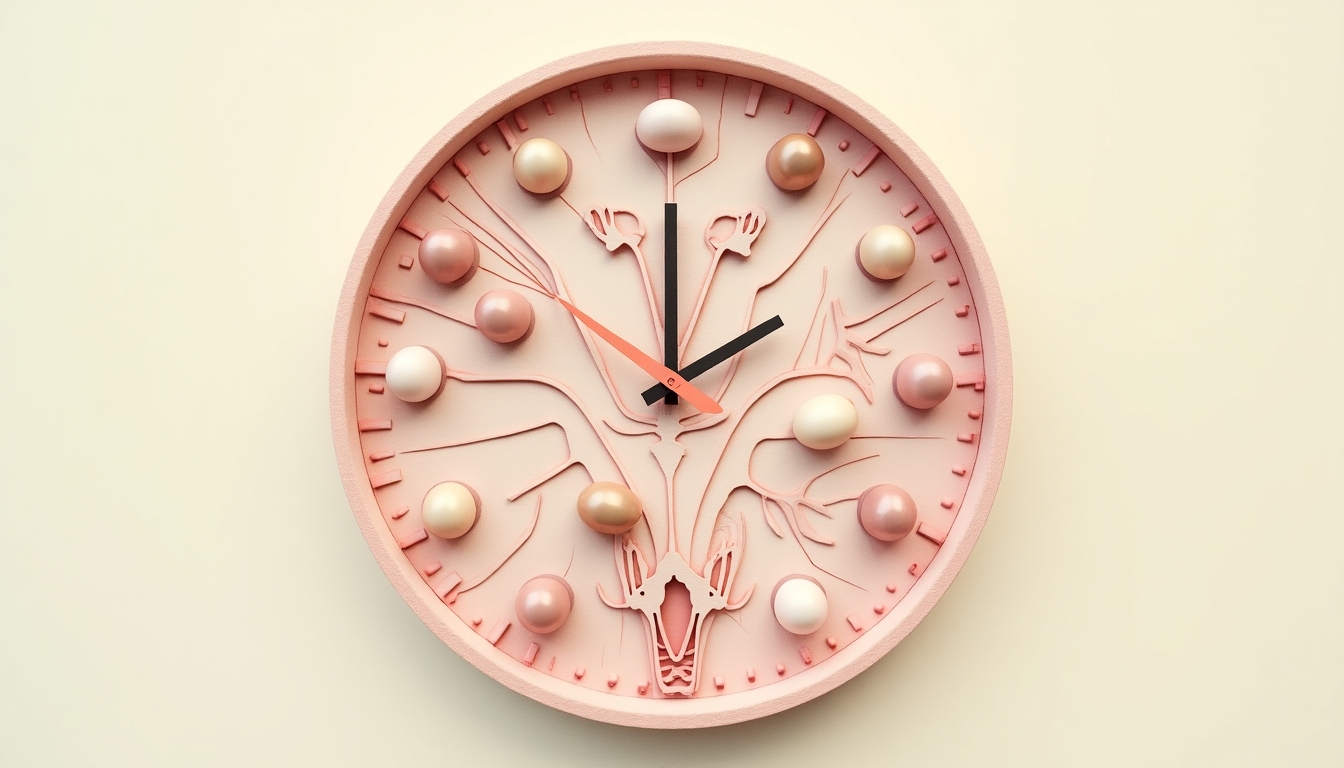
Understanding the Biological Clock: Myths and Facts
March 6, 2025, 7:51 a.m.
The biological clock is a term that often evokes anxiety, especially for women approaching their mid-30s. It refers to the natural decline in fertility that occurs as women age, with a significant drop after 35. This article aims to separate myths from facts, providing a clear understanding of how age impacts fertility and what options are available for women who wish to preserve their fertility. By exploring personal insights and expert knowledge, we hope to empower readers to make informed decisions about their reproductive health.
The biological clock is not just a concept; it's a biological reality rooted in the physiology of human reproduction. Women are born with all the eggs they will ever have—approximately 1 to 2 million at birth. By puberty, this number drops to about 300,000, and only about 300 to 400 eggs will be ovulated during a woman's reproductive years. As women age, not only does the number of eggs decrease, but the quality also diminishes. This decline accelerates after the age of 35, making it harder to conceive and increasing the risk of chromosomal abnormalities in embryos.
There are several myths surrounding the biological clock that can lead to misunderstandings about fertility. Let's explore some prevalent myths and the truths behind them.
- Myth: Women can easily get pregnant in their 40s.
While some women do conceive in their 40s, it's important to understand that fertility declines significantly after 35. According to the Centers for Disease Control and Prevention (CDC), the chance of getting pregnant naturally each month is about 20% for women aged 30, dropping to 5% by age 40.
- Myth: Fertility treatments can overcome age-related infertility.
Fertility treatments like in vitro fertilization (IVF) can assist in conception, but their success rates also decline with age. For women over 40, the success rate per IVF cycle is less than 10%, compared to about 40% for women under 35.
- Myth: Men's fertility doesn't decline with age.
Although men can produce sperm throughout their lives, sperm quality deteriorates with age. Older men may have lower sperm motility and increased DNA fragmentation, which can affect fertility and the health of offspring.

Understanding the facts about the biological clock is crucial for making informed decisions about family planning. Here are some key facts to consider:
- Fertility peaks in the 20s: Women are most fertile between the ages of 20 and 24. After 30, fertility begins to decline gradually, with a steeper drop after 35.
- Increased risks after 35: Women over 35 face higher risks of miscarriage, chromosomal abnormalities, and pregnancy complications such as gestational diabetes and preeclampsia.
- Lifestyle impacts fertility: Factors like smoking, alcohol consumption, diet, and stress can influence fertility. Maintaining a healthy lifestyle can help optimize reproductive health.
For women who are not ready to start a family but wish to preserve their fertility, several options are available:
-
Egg Freezing (Oocyte Cryopreservation)
-
This process involves stimulating the ovaries with hormones to produce multiple eggs, which are then retrieved and frozen. The eggs can be stored for years and later thawed for use in IVF. The success of egg freezing depends on the age at which the eggs are frozen; younger eggs have a higher chance of leading to a successful pregnancy.
-
Embryo Freezing
-
Similar to egg freezing, but the eggs are fertilized with sperm before freezing. This option requires a sperm donor or a partner. Frozen embryos can be stored and transferred to the uterus when the woman is ready to conceive.
-
Ovarian Tissue Freezing
-
This is a less common and more experimental procedure where ovarian tissue is removed and frozen. The tissue can later be transplanted back into the woman to restore fertility. This option is often considered for women undergoing cancer treatments that may affect fertility.

Recognizing the impact of age on fertility is essential for making informed decisions about family planning. Women over 35 who are considering pregnancy should:
- Consult with a fertility specialist to assess their reproductive health.
- Consider fertility testing, such as anti-Müllerian hormone (AMH) levels, to estimate ovarian reserve.
- Discuss options for fertility preservation if they are not ready to conceive immediately.
Navigating fertility and age can be emotionally challenging. Many women feel pressure from societal expectations or personal goals. Sharing stories can help normalize these experiences. For instance, a colleague of mine chose to freeze her eggs at 38 after a breakup, giving her peace of mind while she focused on her career. Another friend started trying to conceive at 36 and faced unexpected difficulties, leading her to explore IVF. These personal journeys highlight the importance of understanding one's options and seeking support.

The biological clock is a reality that affects fertility, particularly for women over 35. By dispelling myths and understanding the facts, women can make informed choices about their reproductive health. Fertility preservation options like egg freezing offer a way to extend the window for having children. It's essential to consult with healthcare professionals and consider personal circumstances when planning for the future.