Long-Term Effects of Ovarian Tissue Freezing: What You Need to Know
April 16, 2025, 5:21 p.m.
Overview
Ovarian tissue freezing is a groundbreaking fertility preservation technique that offers hope to women facing treatments like chemotherapy, which could damage their ovaries and compromise their ability to have children. By freezing ovarian tissue before treatment, women can later have the tissue reimplanted to restore fertility or hormonal function. But what are the long-term effects of this procedure? In this article, we’ll explore the lasting impacts of ovarian tissue freezing on fertility, hormonal health, and overall well-being. Whether you’re considering this option or simply curious about its outcomes, this guide will provide you with the insights you need.
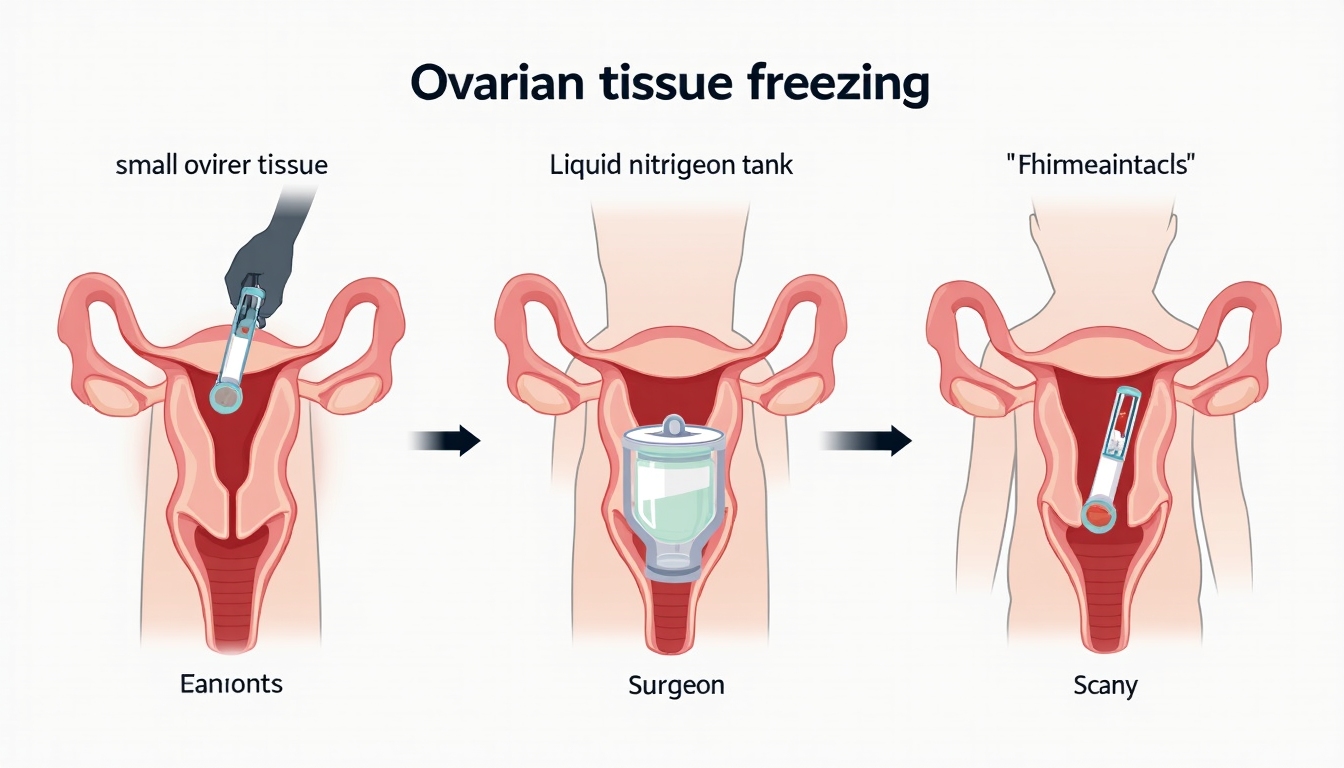
Understanding Ovarian Tissue Freezing
Ovarian tissue freezing involves removing a small piece of the ovary, which contains thousands of immature eggs, and freezing it for future use. This procedure is particularly beneficial for women who need to start cancer treatment quickly and don’t have time for other fertility preservation methods like egg freezing. It’s also an option for young girls who haven’t yet reached puberty. The frozen tissue can be stored for years and, when the patient is ready, transplanted back into her body to restore ovarian function.
Long-Term Fertility Outcomes
One of the most pressing questions for women considering ovarian tissue freezing is whether it will allow them to have children in the future. The good news is that many women have successfully conceived after having their ovarian tissue transplanted back. According to recent studies, the pregnancy rate after ovarian tissue transplantation is around 30-40%, with live birth rates slightly lower but still promising. For example, a 2020 study involving 100 patients reported a 40% pregnancy rate and a 32% live birth rate.
However, the duration of ovarian function after transplantation varies. Some women experience restored fertility for several years, while others may have a shorter window. On average, the transplanted tissue functions for about 4-5 years, but this can depend on factors like the patient’s age at the time of freezing and the quality of the tissue.
Here’s a quick look at some key statistics from recent studies:
| Study Year | Number of Patients | Pregnancy Rate | Live Birth Rate |
|---|---|---|---|
| 2015 | 50 | 30% | 25% |
| 2018 | 75 | 35% | 28% |
| 2020 | 100 | 40% | 32% |
While these numbers are encouraging, it’s important to note that ovarian tissue freezing is still a relatively new technique, and long-term data is still being collected. Compared to other fertility preservation methods like egg freezing, which has been around longer, ovarian tissue freezing offers unique advantages, especially for prepubertal girls or women who need immediate treatment.

Hormonal Health and Menopause
Beyond fertility, ovarian tissue freezing can also play a crucial role in restoring hormonal function. The ovaries produce hormones like estrogen and progesterone, which are essential for regulating the menstrual cycle and maintaining bone health. For women who undergo early menopause due to cancer treatments, transplanting frozen ovarian tissue can help restore these hormones, delaying menopause and reducing symptoms like hot flashes or osteoporosis.
However, the long-term hormonal benefits are not guaranteed. Some women may experience a temporary restoration of ovarian function, while others may have longer-lasting effects. Research suggests that hormonal function can be maintained for several years post-transplant, but it often declines over time as the tissue ages.

Risks and Complications
Like any medical procedure, ovarian tissue freezing and transplantation come with potential risks. One of the most significant concerns is the possibility of reintroducing cancer cells if the tissue was frozen before cancer treatment. This risk is particularly relevant for cancers like leukemia, which can affect the ovaries. To mitigate this, doctors carefully screen the tissue before transplantation, but the risk can never be entirely eliminated.
Other risks include: - Surgical complications: Both the removal and transplantation of ovarian tissue involve surgery, which carries risks like infection or bleeding. - Graft failure: In some cases, the transplanted tissue may not function as expected, leading to limited or no restoration of fertility or hormonal function. - Long-term health effects: While rare, there may be unknown long-term health implications, as the technique is still relatively new.

Psychological and Emotional Aspects
The decision to undergo ovarian tissue freezing is often made during an already stressful time, such as a cancer diagnosis. This can take an emotional toll on patients, who may feel overwhelmed by the uncertainty of their future fertility. Additionally, the waiting period between freezing the tissue and eventually using it can be anxiety-inducing, as women wonder whether the procedure will work when they’re ready to start a family.
On the positive side, many women report feeling empowered by taking control of their fertility. Knowing that they have a backup plan can provide peace of mind during treatment and recovery. Support from family, friends, and counseling services can also play a crucial role in helping women navigate the emotional aspects of this journey.

Advancements and Future Prospects
Ovarian tissue freezing is still evolving, with ongoing research aimed at improving its success rates and expanding its applications. Recent advancements include better cryopreservation techniques, which help preserve the tissue’s viability, and the development of artificial ovaries, which could one day eliminate the need for transplantation altogether.
In the future, this technique may be used not only for cancer patients but also for women who want to delay childbearing for personal or medical reasons. As more long-term data becomes available, we’ll have a clearer picture of the procedure’s lasting effects and potential.
Summary
Ovarian tissue freezing offers a promising option for fertility preservation, with many women successfully conceiving after transplantation. However, it’s not without risks, and the long-term effects on hormonal health and overall well-being should be carefully considered. If you’re facing a situation where fertility preservation is a concern, consult with a reproductive specialist to discuss your options. While the technique is still relatively new, ongoing research and advancements continue to improve its outcomes, offering hope to women worldwide.