How IVF Processes Have Evolved Over the Decades
March 11, 2025, 7:53 a.m.
In the realm of reproductive medicine, few innovations have been as transformative as In Vitro Fertilization (IVF). Since its inception, IVF has not only revolutionized the way we approach infertility but has also opened new avenues for fertility preservation. This article delves into the evolution of IVF processes over the decades, highlighting key advancements, the rise of fertility preservation techniques, and the profound impact these developments have had on individuals and families worldwide.

The story of IVF begins in the late 1970s with the birth of Louise Brown, the world's first "test-tube baby." This groundbreaking event marked the culmination of years of research and experimentation by pioneers like Dr. Robert Edwards and Dr. Patrick Steptoe. However, the early days of IVF were fraught with challenges, including low success rates and ethical controversies. Despite these hurdles, the promise of IVF as a solution for infertility spurred continued innovation and refinement.

As the 1980s and 1990s progressed, significant advancements were made in IVF techniques. One of the most notable was the development of ovarian stimulation protocols, which allowed for the production of multiple eggs, thereby increasing the chances of successful fertilization. This was a game-changer, as it addressed one of the primary limitations of early IVF— the low yield of viable eggs. Additionally, the introduction of intracytoplasmic sperm injection (ICSI) in the early 1990s revolutionized the treatment of male infertility. ICSI involves the direct injection of a single sperm into an egg, bypassing many of the barriers that previously made fertilization impossible for men with severe sperm abnormalities.
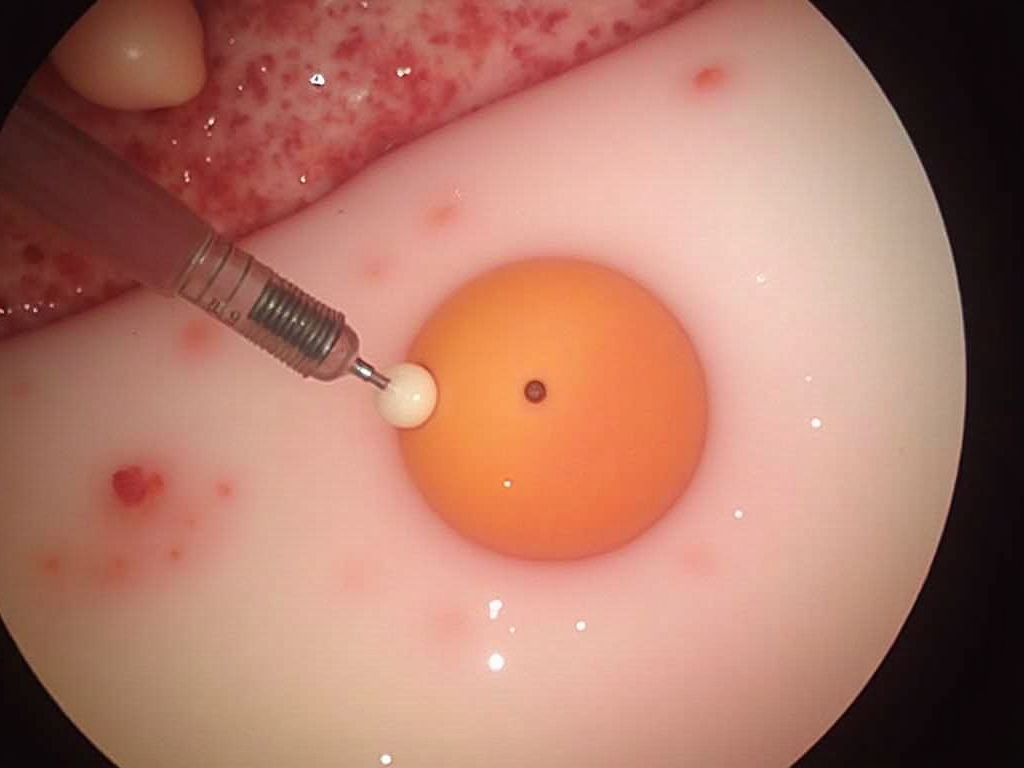
The turn of the millennium brought further refinements to IVF processes, particularly in the realm of embryo culture and selection. Improved culture media, designed to mimic the natural environment of the fallopian tube, allowed embryos to develop more robustly in the lab. The advent of time-lapse imaging enabled embryologists to monitor embryo development continuously without disturbing the culture conditions, leading to better selection of the most viable embryos for transfer. Moreover, the emergence of preimplantation genetic testing (PGT) enabled the screening of embryos for genetic abnormalities, reducing the risk of inherited disorders and increasing the likelihood of a healthy pregnancy. PGT has since evolved to include not only the detection of chromosomal abnormalities but also the identification of specific genetic mutations.

Parallel to these advancements in IVF, the field of fertility preservation has also seen remarkable progress. Initially developed for cancer patients facing treatments that could compromise their fertility, fertility preservation techniques such as egg and sperm freezing have become increasingly sophisticated. For women, oocyte cryopreservation (egg freezing) has become a popular option, allowing them to preserve their fertility potential for future use. Similarly, sperm freezing has long been a reliable method for men. More recently, ovarian tissue freezing and transplantation have emerged as experimental but promising techniques for preserving fertility in prepubertal girls and women who cannot delay cancer treatment.

The success rates of fertility preservation have improved significantly over the years, thanks to advancements in cryopreservation technology. Vitrification, a rapid freezing technique that prevents the formation of ice crystals, has largely replaced older slow-freezing methods. This has resulted in higher survival rates for frozen eggs and embryos, making fertility preservation a more viable option for many. According to recent studies, the success rates for IVF using vitrified eggs are now comparable to those using fresh eggs, with pregnancy rates exceeding 50% in some cases. This has been a boon for individuals seeking to delay parenthood for personal or professional reasons, as well as for those facing medical treatments that could impact their fertility.
The evolution of IVF and fertility preservation has not been without its ethical and social considerations. In the early days, IVF faced significant opposition from various quarters, including religious groups and bioethicists. However, as the technology matured and its benefits became more apparent, societal attitudes shifted. Today, IVF is widely accepted, and discussions around fertility preservation often center on issues of accessibility and equity.

In the current landscape, IVF continues to evolve with the integration of cutting-edge technologies such as artificial intelligence and machine learning. These tools are being used to optimize embryo selection, predict treatment outcomes, and personalize patient care. Additionally, research into areas like mitochondrial replacement therapy and stem cell-derived gametes holds promise for addressing previously untreatable forms of infertility.
Throughout its history, IVF has been more than just a medical procedure; it has been a source of hope and a testament to human resilience. Personal stories of individuals and couples who have navigated the challenges of infertility with the help of IVF underscore the profound impact of this technology. From the joy of welcoming a long-awaited child to the empowerment of preserving fertility options, these narratives highlight the human side of IVF's evolution.

In conclusion, the journey of IVF from its experimental beginnings to its current status as a cornerstone of reproductive medicine is a remarkable tale of scientific progress and human determination. As we look to the future, the continued evolution of IVF processes and fertility preservation techniques promises to further expand the possibilities for individuals and families facing infertility. With each advancement, we move closer to a world where the dream of parenthood is within reach for all.